The Republics of Botswana and Zambia have made steady progress toward achieving the 95-95-95 targets. Both teach us several lessons for combating HIV and the clear leadership role of the U.S. President’s Emergency Plan for AIDS Relief (PEPFAR):
- Granular data – disaggregated by age, sex, and geography – are critical for success and should be used to act on challenges in a timely fashion.
- Access to and adoption of services across all population groups is key.
- Data-driven policy changes and their rapid implementation across all health institutions are crucial.
- HIV services integrated into community clinics must be well-staffed, nondiscriminatory, and accessible to everyone.
- Data validation is crucial to create programming that rapidly addresses gaps in care.
- Sustained political will and domestic resource mobilization are essential to continued innovation and progress.
Botswana: Fulfilling the promise of treatment for all
Almost 40% of people in Botswana were living with HIV 20 years ago, threatening the country’s very survival. Forty percent of pregnant women had unknowingly transmitted the virus to their babies. Even as the government boldly committed to making treatment available to everyone, Botswana faced significant challenges, including outdated policies and shortages of medical personnel in a geographically large country with a dispersed population. Additionally, social stigma discouraged many people – especially men – from getting tested in HIV centers and clinics.
The government and local communities responded by reinventing the delivery of HIV prevention, care, and treatment. Testing for HIV became routine; today, even at-home self-testing is widely available. The government adopted new drug regimens with fewer side effects that required fewer follow-up visits. Mobile clinics reach the most rural populations; HIV-specific counselors and services are integrated into community clinics; and nurses and doctors share more responsibilities. These reforms have made HIV care more cost effective and accessible for everyone, regardless of HIV status. Between 1999 and 2020, the rate of mother-to-child transmission of HIV in Botswana declined by 87%.
Constant monitoring and evaluation across districts and communities allows the government of Botswana and its partners – including PEPFAR, civil society, and other donors – to track progress successfully and create effective programming based on real-time data. When the 2013 national HIV survey funded by PEPFAR showed men were lagging behind in early diagnosis and treatment, the government redoubled its efforts with communities and churches to ensure more men had access to and kept up with treatment. As a result, the next survey completed in 2021 showed that the overall percentage of people living with HIV had fallen to 20%.
Botswana’s emphasis on data-driven screening and treatment has yielded dramatic results. More than 339,000 people were on antiretroviral therapy (ART) in Botswana in 2023, compared with approximately 159,000 in 2010, and the number of annual new HIV infections has declined by 80% since PEPFAR’s inception in 2003 (Figure 3).
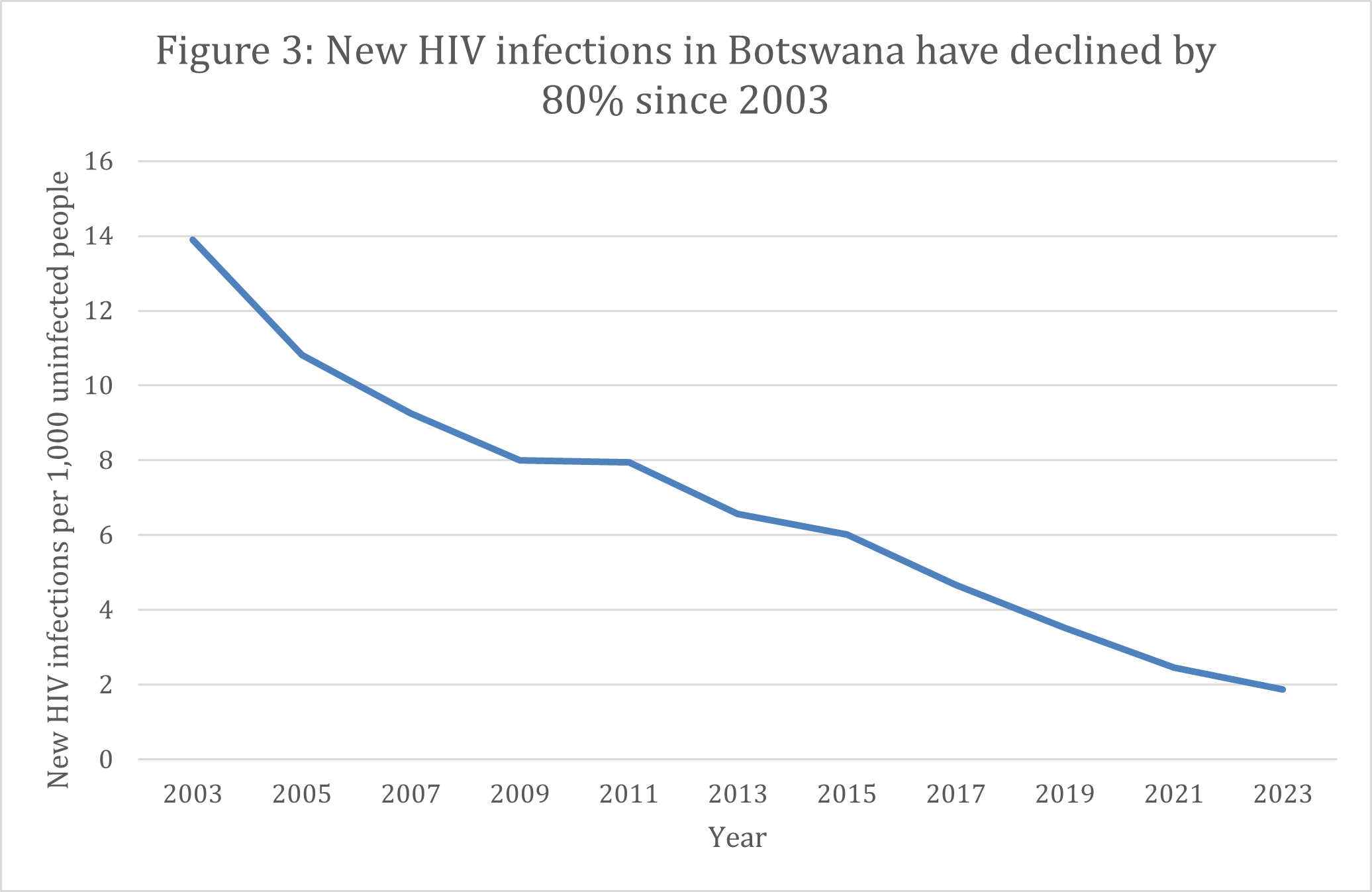
Source: UNAIDS
Botswana is a leader among countries on track to reach the 95-95-95 goals, and the national government funds a greater percentage of its HIV response each year. This cost-effective model of engaging the community and using data to find and address gaps in care demonstrates that the right policy changes can dramatically change the course of HIV infections and treatment. Beyond 2030, Botswana serves as a lesson for national governments’ responses to chronic diseases.
| The Republic of Botswana | ||
| At least 95% of all people living with HIV should know their status (as of 2023) | At least 95% of all people with diagnosed HIV should receive ART and continue it (as of 2023) | At least 95% of all people on ART should have undetectable levels of the virus in their blood, known as viral load suppression (as of 2023) |
| >95% | 95% | 94% |
Zambia: Innovation in the face of disaster
Zambia tells a similar story of dedication, adaptation, and innovation. By the early 2000s, approximately one in six Zambians were living with HIV. Trucking routes between some of the richest mines in the world and the ports of southern Africa allowed HIV to spread quickly through the country. However, public health care and investments were concentrated in the country’s capital, leading to significant resource gaps and inefficiencies in rural areas.
Today, with over 20 years of strong technical and financial support from PEPFAR and the Global Fund to Fight AIDS, Tuberculosis, and Malaria, Zambia has become a model for HIV response by using data to constantly improve programs and address gaps in access. Since the rate of HIV infection varies greatly between geographies and ages in Zambia, each province is adapting to the specific needs of its communities – an innovative change from a one-size-fits-all approach. Decentralizing much of the national health budget to the provinces allows for a nimbler response to HIV and directs resources to populations with the greatest need.
Much like Botswana, Zambia has also expanded the ways patients receive treatment. Doctors, nurses, and community health workers share tasks and trade roles when needed. Community clinics and mobile units have brought care and ART directly to the people, ensuring they maintain strict medicine regimes.
A hallmark of Zambia’s response has been the rapid adoption and uptake of HIV prevention approaches. It was one of the first countries to introduce preexposure prophylaxis (PrEP) – drugs that can prevent someone from contracting HIV – including long-acting PrEP in 2024. The Zambian government and its partners have worked closely with PEPFAR to provide opportunities for young girls to prevent early sexual activity through the Determined, Resilient, Empowered, AIDS-Free, Mentored, and Safe (DREAMS) program. Finally, the successful adoption of voluntary male medical circumcision (VMMC) has reduced the risk of HIV acquisition for hundreds of thousands of men.
The latest PEPFAR-funded Zambia Population-Based HIV Impact Assessment (PHAI), conducted in 2021, shows that the overall percentage of people infected with HIV in Zambia between April and December of that year declined to 11%. PEPFAR’s partnership and Zambia’s policy changes have led to an 80% decline in annual new HIV infections since 2003 (Figure 4). And Zambia is on track to reach the 95-95-95 goals.
|
The Republic of Zambia |
||
| At least 95% of all people living with HIV should know their status (as of 2023) | At least 95% of all people with diagnosed HIV should receive ART and continue it (as of 2023) | At least 95% of all people on ART should have undetectable levels of the virus in their blood, known as viral load suppression (as of 2023) |
| >95% | 95% | 92% |
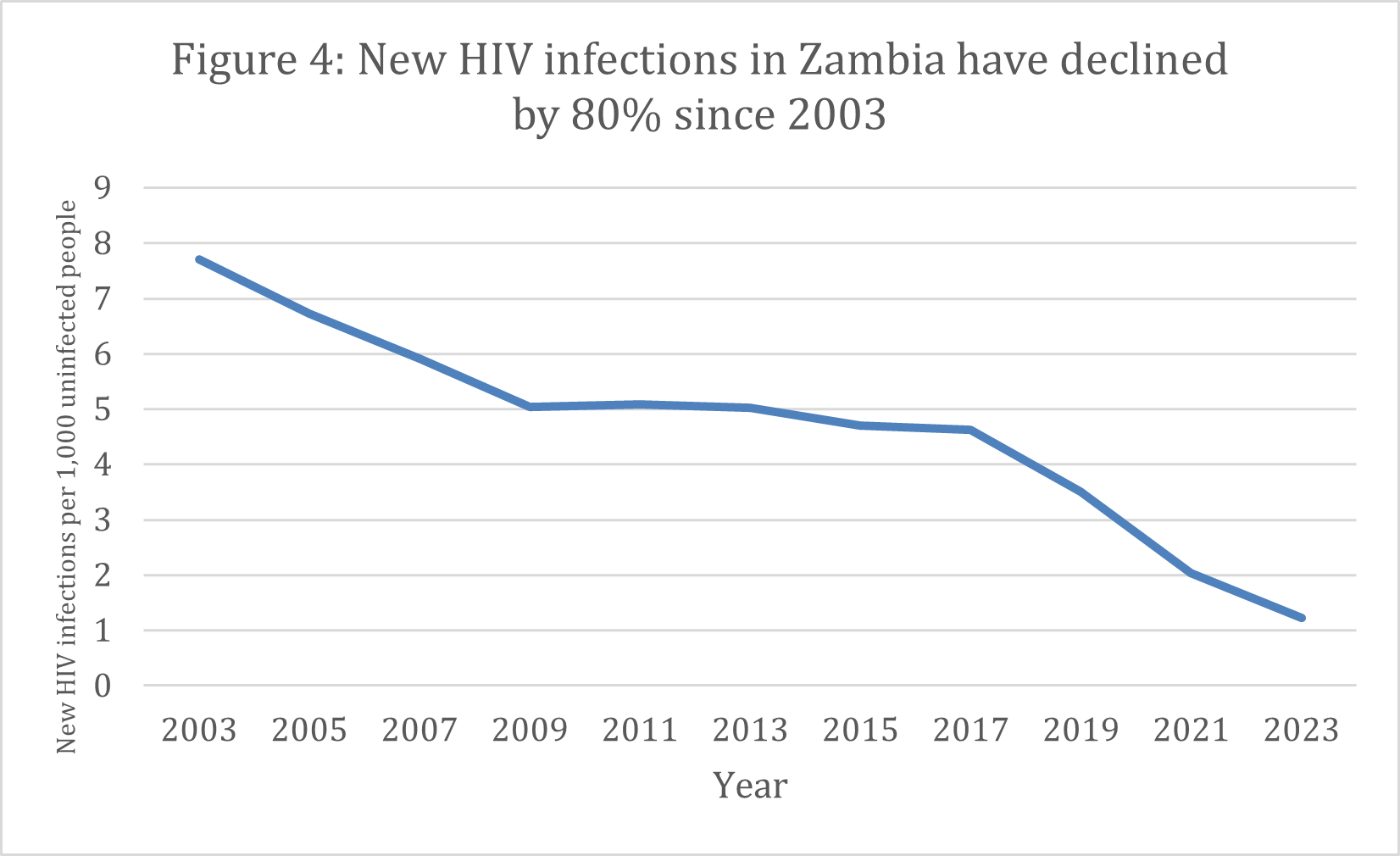
Source: UNAIDS
Sustaining this progress will require persistent monitoring of treatment and viral load suppression and access to long-acting PrEP for the most-at-risk groups. A key lesson learned from Zambia’s progress is the need to validate programmatic data on an ongoing basis with independent surveys. The first Zambia PHIA in 2016 showed a significant discrepancy in the numbers of people on treatment reported by PEPFAR and the national government. After a full data-quality assessment revealed that the program was double-counting clients, PEPFAR and the Zambian government worked together to strengthen reporting and data collection, leading to a correction (Figure 5).
Figure 5: Number of new people in Zambia on treatment with PEPFAR support
Source: PEPFAR
*Year reflects U.S. government fiscal year
Strict data and reporting mechanisms will be essential to ensuring future success in Zambia. The PEPFAR team, the community, and the government must carefully watch the retention of clients on ART. A decline in the net new number of patients on treatment because some are dropping out of care (known as loss to follow-up) is an early-warning signal of programmatic gaps that need urgent solutions. Understanding precisely who is out of care and why and addressing these barriers through community and peer support will be essential to maintaining Zambia’s low rates of new HIV infections. Interoperable electronic medical records and unique identifiers can alleviate these challenges. Zambia’s data-driven programming provides the foundation for a strategic approach to other chronic diseases and the response to any future pandemics.
































