It Takes a System
There are no shortages of health care problems, even crises, such as the COVID-19 pandemic. But they are best addressed through creating strong systems to care for people in need.
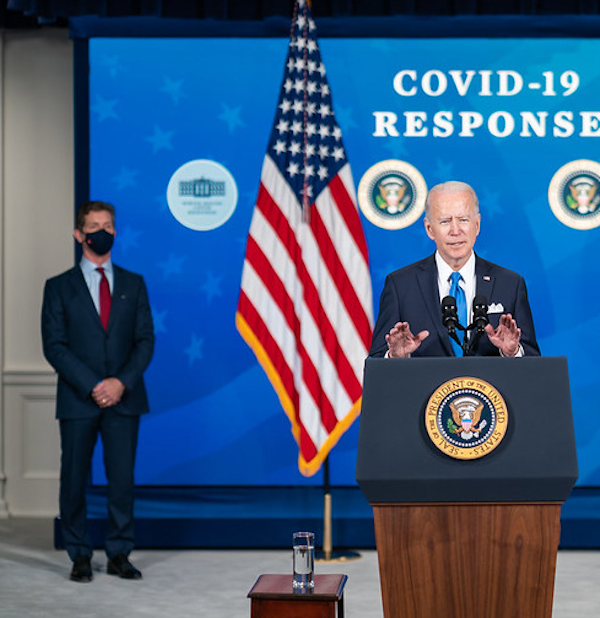 President Joe Biden, joined by Johnson & Johnson CEO Alex Gorsky, delivers remarks on COVID-19 vaccine production on March 10, 2021. (The White House/Flickr)
President Joe Biden, joined by Johnson & Johnson CEO Alex Gorsky, delivers remarks on COVID-19 vaccine production on March 10, 2021. (The White House/Flickr)
Alex Gorsky, the April and Jay Graham Fellow at the Bush Institute, is the former Chairman and CEO of Johnson & Johnson. The West Point graduate, who has worked on health care challenges both in the United States and around the world, spoke with The Catalyst about the importance of strong systems in tackling major health care problems.
Addressing those issues requires business and government working together, including to respond to crises such as the spread of AIDS or the sudden onslaught of the COVID-19 pandemic. As the longtime health care executive notes, collaboration takes a willingness to understand each other’s priorities and approaches to a problem. In the end, though, people in need will be best served.
What have you learned from your efforts in the private and public arenas to address significant health care challenges, whether that’s improving care for veterans, dealing with the COVID pandemic domestically, or addressing AIDS globally?
The first thing I would like to note is that we’ve learned the importance of having strong, robust global public health policies and systems in place. Particularly with COVID-19, we’ve learned that our larger society, national security, and economy are at risk if we don’t have those kinds of systems in place.
Making sure that we put the time, energy, effort, and resources into these systems is more important than ever. Not only does it matter at a global or national level, but it’s important at a personal level. Ultimately, those systems touch each one of us as an individual and as a family member, whether as a mom, dad, sister, or brother.
The first thing I would like to note is that we’ve learned the importance of having strong, robust global public health policies and systems in place.
Next, it’s fundamental to always start with an innovative mindset. It’s not just about doing things faster or more efficiently. But how do we try to harness science or the many emerging new technologies? How do we put them to use in a positive way to make a difference?
We’re seeing pretty significant progress in all these areas. When I first started in this industry more than 35 years ago, if one was diagnosed with HIV, on average, they might have two years to live. Today, treated in the right way, patients can have maybe two years taken from their average lifespan. That’s a remarkable achievement.
Similarly, we found with COVID-19 that had we not been investing for decades in new technologies like mRNA, we would never have been in our current position. So, it’s important to use innovation in the right way to not only address an issue but also to get access to care. You need that mindset from the start.
 Innovation of Johnson and Johnson COVID-19 vaccines in 2021. (Photo Courtesy of Shutterstock)
Innovation of Johnson and Johnson COVID-19 vaccines in 2021. (Photo Courtesy of Shutterstock)
How the public sector and private sector can work together also matters. Neither side has all the answers. But you can make magic happen when you take the business approach — speed to innovation, sense of urgency, and utilizing multiple networks – and put it together with the resources, size, and scale of governments.
Whether it’s PEPFAR, COVID-19, or even in veterans’ initiatives, we have operated at our best when we brought together the best practices from business and government behind a common cause. We then can produce a meaningful, sustainable outcome.
You’ve spent most of your time on the private side, but what lessons have both sides learned through their collaborative work on these various health challenges?
We’ve learned a lot. It starts with learning each other’s language.
If you get a bunch of business people around, they’ll often start with a certain perspective, a certain construct, and the government people will use a multitude of acronyms coming from the government. Making sure that you’re aligned behind common objectives and trying to find the language to accurately describe what we’re actually trying to do is so important.
You can make magic happen when you take the business approach – speed to innovation, sense of urgency, and utilizing multiple networks – and put it together with the resources, size, and scale of governments.
Next, it’s trying to understand the constraints and constructs that each other works under. I realize that it can be frustrating for individuals in business to deal with a very large bureaucracy. But that’s part of the reality. And if you don’t try to understand that, and take the time to learn how decisions get made in the government, you’ll never pass some of the policies, programs, or initiatives that you’d like to get through. That takes an investment of time, energy, and effort.
At the same time, it’s incumbent upon our government officials to make an extra effort to reach out to businesses and realize the constraints that they operate under. It could be frustrating for government officials because they’re looking at an issue from a U.S. point-of-view whereas a company may be a global organization. It’s not that the businesses are not patriotic or committed to the United States, but it’s understanding the ramifications that can happen outside of our particular borders.
These are a few examples of the issues and challenges, but there also are opportunities in public-private partnerships.
I’d like to tease out a bit more where you see these systems leading to success.
What I’ve seen directly lead to success is harmonizing the efforts of researchers, business, and regulators and aligning them behind a common objective. I want to be clear that this did not take any shortcuts. It reinforced many of the principles of science and process that we had in place.
But what made a radical difference in the timelines around the discovery and development of COVID-19 vaccines was being able to do some of these things in parallel versus in a sequential approach that you might normally take.
Next, it’s fundamental to always start with an innovative mindset. It’s not just about doing things faster or more efficiently. But how do we try to harness science or the many emerging new technologies? How do we put them to use in a positive way to make a difference?
We’ve seen similar approaches in some of the medical breakthroughs in treating veterans. Have a sense of urgency to do everything we can to help them, but also try to simplify some of the processes and systems that tend to work against each other. Getting them behind the common goal is important.
It’s also a question of how you achieve scale. It’s one thing to have a single product approved, but how do you distribute that to thousands of people? How do you make sure you can go that last mile from the laboratory to the actual patient? If you’re treating an HIV patient, helping that veteran directly, or as we found in overcoming skepticism about the COVID-19 vaccine, you can’t have the desired impact if you don’t get that last mile right.
 Truvada is a prescription medication used to prevent and treat HIV infection. (Antwon McMullen/Shutterstock)
Truvada is a prescription medication used to prevent and treat HIV infection. (Antwon McMullen/Shutterstock)
You like to talk about increasing health for the whole person. How do you see systems doing that? Do other challenges stand in the way?
Some of the challenges we face in health care reflect the challenges that we face more broadly as a society. They tend to manifest themselves in the health care system. So, if we’re not providing the right kind of education and information on things like diet and behavior, which play an important factor in our overall health care outcomes, we will always be chasing our tails, so to speak, in many of these issues.
I, for one, would like to see us invest more in prevention than just the treatment of certain conditions.
More and more, we realize that 75% of the things that affect us and usually lead to death can be directly attributable to our behaviors. It might be diet, activity level, sleep. Or it might be getting vaccinated in certain periods of time or how we access the health care system. All of these have a tremendous impact on long-term outcomes and actual health care utilization.
I, for one, would like to see us invest more in prevention than just the treatment of certain conditions. And we all know that if we get to certain diseases earlier, whether it’s cardiovascular disease or certain types of cancers, we can predict much better outcomes and get better interventions into place.
Now, that requires not only prevention but also equitable access to our health care system. Breaking down barriers to that system has so much potential, whether it’s in underserved communities, rural communities, or for veterans. We can have a better impact on veterans, patients, and, frankly, all of our U.S. citizens.
The Catalyst believes that ideas matter. We aim to stimulate debate on the most important issues of the day, featuring a range of arguments that are constructive, high-minded, and share our core values of freedom, opportunity, accountability, and compassion. To that end, we seek out ideas that may challenge us, and the authors’ views presented here are their own; The Catalyst does not endorse any particular policy, politician, or party.
-
Previous Article We Need to Explore Psychedelic-Assisted Therapy for Veterans Interview with Margaret Harrell, Chief Program Officer at the Bob Woodruff Foundation, and Colonel Matthew Amidon, Former Director of Veterans and Military Families at the George W. Bush Institute
-
Next Article Addressing Period Poverty Will Expand Access to Health Care Essay by Robert A. McDonald, Former U.S. Secretary of Veterans Affairs and Former President and CEO of Procter & Gamble

